Request an appointment by submitting UofL Health’s appointment request form or calling our clinic at 502-588-2160. When requesting an appointment, please note our specialty is neurosurgery and our brain bypass providers are Dr. Josh Abecassis and Dr. Dale Ding.
UofL Health’s Louisville Brain Bypass and Revascularization Center (LBBRC) aims to identify and treat patients with Moyamoya disease (MMD), Moyamoya syndrome (MMS), related intracranial steno-occlusive disorders (SOD), and extracranial vascular stenosis (carotid and vertebral) with medical and surgical treatment options. Our team evaluates each patient through a comprehensive, interdisciplinary program of UofL Health providers spanning multiple neuro-specific subspecialties.
Conditions and conditions treated:
- Moyamoya Disease (MMD): This is a progressive narrowing of the intracranial carotid arteries, usually with one side first followed by the other, and progressive strokes, transient ischemic attacks (TIAs, or “mini-strokes”), and/or bleeds in the brain.
- Moyamoya syndrome (MMS): MMS is like MMD but more often affects one side of the brain only. It can be associated with a number of conditions like lupus, prior radiation, sickle cell anemia, Down syndrome, neurofibromatosis, or thyroid disease, or it can present due to unknown reasons (i.e. “idiopathic”). Similar to MMD, MMS can present with progressive strokes, transient ischemic attacks (TIAs, or “mini-strokes”), and/or bleeds in the brain.
- Steno-occlusive disorders (SOD): SOD includes any narrowing or closed arteries in the brain, which can happen for various reasons including dissections, tears in the artery, or a build-up of plaque (i.e. intracranial atherosclerotic disease (ICAD)). Most of the time, medical management is best for first-line treatment.
- Carotid or vertebral artery stenosis: Narrowing in the blood vessels of the head and neck, and can present with strokes or TIAs. A combination of medical and/or surgical treatment is used for these patients.
Treatments and procedures we offer:
Medical Management: We have experts in vascular neurology that will evaluate each patient for any and all risk factors associated with disease progression and – when appropriate – develop a personalized regimen of medication with close appointment follow-up. This includes anti-platelet medication, anti-coagulation (blood thinners), cholesterol and hypertension-modifying medications, along with lifestyle modification.
Endovascular options: Most patients will undergo a diagnostic angiogram using wires and catheters, through either the wrist or groin artery, to evaluate the blood vessels of the brain, head, and neck. This procedure is performed generally as an outpatient appointment and takes about an hour, with 1-4 hours of recovery before discharge. Since this procedure involves entering the arteries of the head and neck, it is classified as invasive and therefore has a small risk of causing a stroke. We take every precaution possible to prevent this and the risk of stroke is less than 1%. This procedure is generally required for a thorough evaluation of the blood vessels.
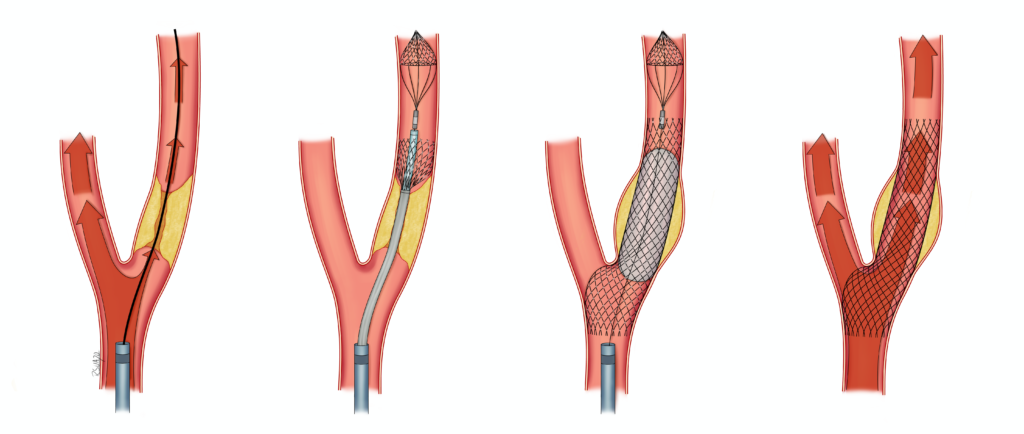
- Stent: In some cases of SOD or carotid or vertebral stenosis, endovascular stenting may be an option to enhance blood flow to the brain. Any stenting requires that the patient take 2 separate antiplatelet medications (usually aspirin and Plavix) for 6 months, and a single antiplatelet agent thereafter.
Surgical options:
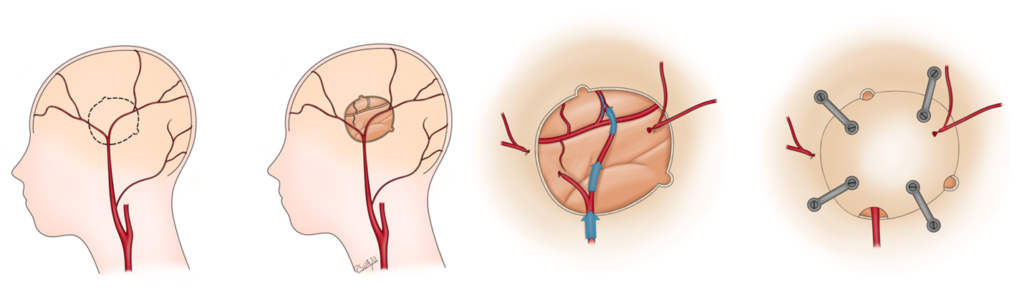
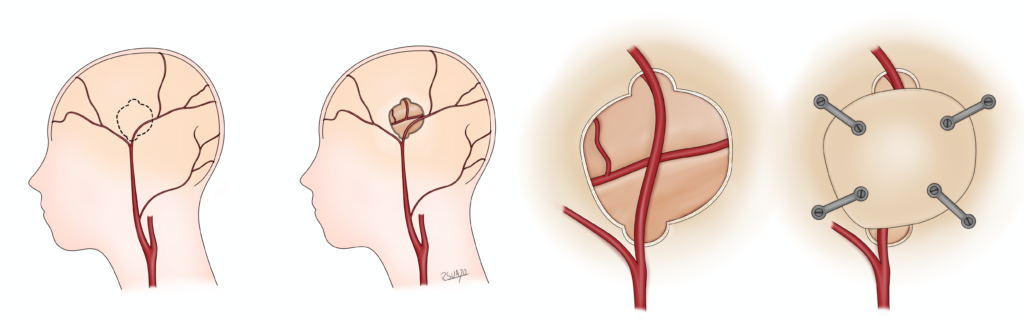
- Bypass (Direct): One way to restore blood flow to the brain is to use an artery that normally goes to the scalp (either the superficial temporal artery (STA) or occipital artery) and connect it to a brain blood vessel after performing a craniotomy. This procedure is called a “direct bypass”. This procedure does require both the donor scalp blood vessel and recipient brain blood vessel to be of sufficient size. The most common donor is the superficial temporal artery (STA) and the most common recipient is the middle cerebral artery (MCA) of the brain, this form of direct bypass is called an “STA-MCA bypass”. STA-MCA bypass is the preferred treatment for patients with MMS and MMD (where there is no known medical or endovascular treatment option shown to help patients). Very rarely, we use an artery in the arm (radial artery) or leg (tibial artery) to connect the carotid artery in the neck to the blood vessels of the brain to supply more blood flow. We are the only center in the state and one of the few in the region to offer direct bypasses to patients. Patients with this surgery take a full dose of aspirin for approximately 1 year and then decrease to baby aspirin thereafter.
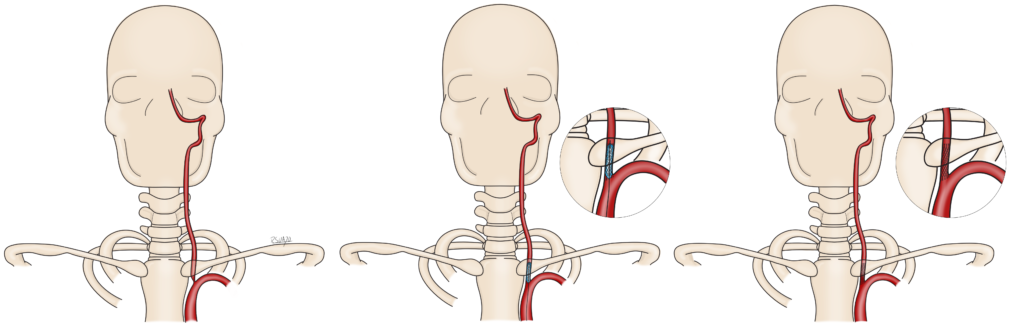
- Indirect revascularization: If the recipient or donor blood vessels are not viable or large enough to perform a direct bypass, we can perform an indirect revascularization procedure where a piece of scalp tissue (muscle, the STA, etc.) or meninges is laid on top of the brain after performing craniotomy for blood vessels to grow over time and help flow to the brain. This procedure also has excellent results in preventing strokes and TIAs in patients with MMS and MMD.
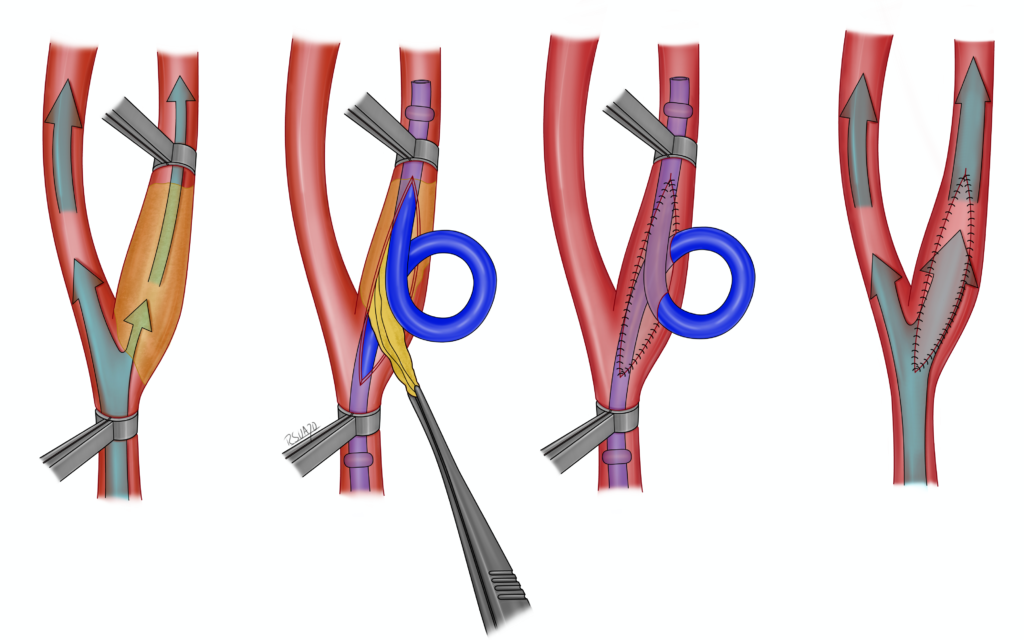
- Carotid endarterectomy: For carotid stenosis in the neck, oftentimes we can offer surgery to open the carotid artery in the neck and remove the plaque to reduce the risk of having a stroke or TIA. For patients with carotid stenosis, each case is different, and we will discuss the benefits and risks of both using a stent and surgical removal of the plaque.