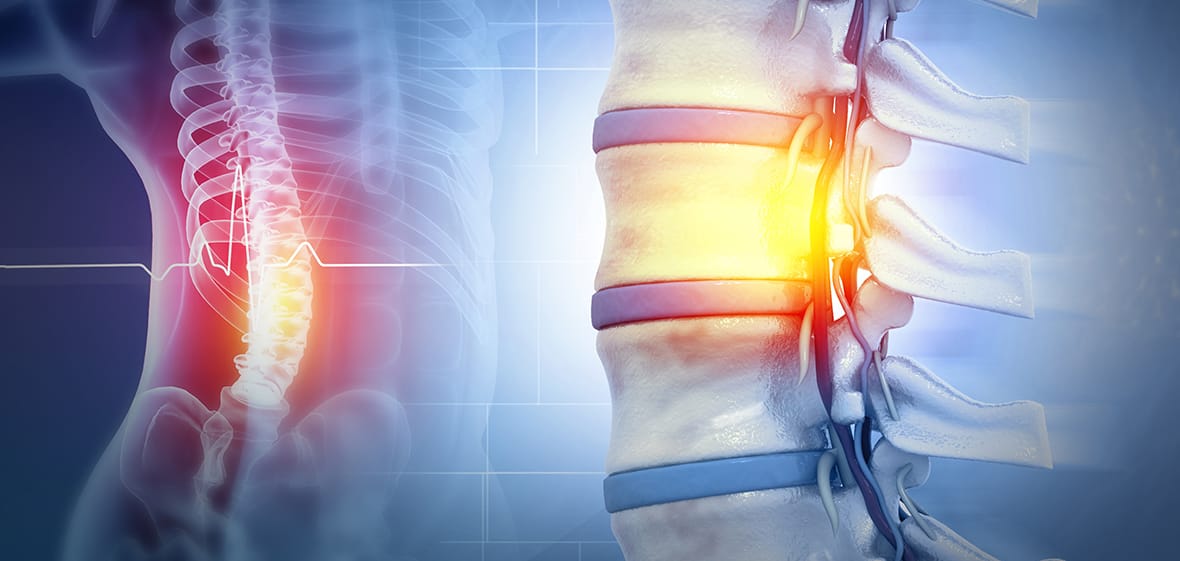
Spinal cord injuries (SCIs) are among the most life-altering conditions a person can experience. The spinal cord is not just a conduit for motor and sensory signals—it’s a critical communication highway between the brain and the rest of the body. When this pathway is disrupted, the consequences can be profound.
What Defines an SCI?
An SCI occurs when trauma or disease damages the spinal cord or its surrounding structures, impairing the transmission of nerve signals. These injuries can result in varying degrees of motor, sensory and autonomic dysfunction, depending on the location and severity of the injury.
Common causes include:
- Motor vehicle accidents
- Violence
- Falls
- Diving into shallow water
- Sports-related trauma
No two spinal cord injuries are identical, and the clinical presentation can vary widely—even among patients with similar injuries.
Complete vs. Incomplete SCI: What’s the Difference?
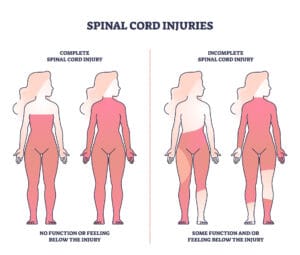
Complete SCI
A complete SCI is characterized by a total loss of motor and sensory function below the level of injury. This means the spinal cord has been severely damaged to the point where no signals can pass through. Patients with complete injuries typically present with:
- No voluntary movement or sensation (pain, temperature, touch) below the level of injury, including the rectal area.
- No autonomic function (e.g., bowel or bladder control).
Incomplete SCI
An incomplete SCI, which is more common, involves partial preservation of sensory or motor function below the level of injury. The spinal cord may be compressed, bruised or partially damaged, but some neural pathways remain intact. These patients may still have:
- Partial movement or strength, as well as some degree of sensation below the level of injury, including the rectal area.
- Variable autonomic function.
The extent of retained function can vary significantly, and classification often depends on a detailed and specific neurological examination and imaging.
Determining the Type of Injury
Shortly after the injury, distinguishing between complete and incomplete SCI can be challenging. Swelling, bleeding and spinal shock may temporarily mask function. Over time, as inflammation goes away, a clearer picture emerges.
Clinical evaluation includes:
- Neurological examination using the International Standards for Neurological Classification of Spinal Cord Injury, also known as the “ASIA exam”
- MRI to assess structural damage
- Monitoring for return of function over days to weeks
If a patient demonstrates any motor or sensory function below the level of injury, the SCI is considered incomplete—a more promising sign for potential recovery.
Is Recovery or Adaptation Possible After an SCI?
Recovery from an SCI—whether complete or incomplete—is a complex and deeply personal journey. While complete SCIs often result in permanent loss of function below the level of injury, advances in rehabilitation, assistive technology and neuroplasticity research continue to expand what’s possible. Incomplete injuries, which preserve some motor or sensory function, offer a broader range of recovery potential.
However, recovery isn’t the only path forward. Adaptation—learning new ways to navigate life, build independence and find purpose—is equally vital. Many individuals with SCIs go on to lead fulfilling lives, pursuing careers, relationships, hobbies and personal goals with resilience and determination.
Whether through intensive therapy, adaptive equipment or community reintegration strategies, the goal is clear: to help individuals live fully, regardless of the extent of their injury.
The Spinal Cord Program at UofL Health – Frazier Rehabilitation Institute is nationally recognized for its innovative, patient-centered approach. Through advanced therapies and a unique multidisciplinary team—including nurse navigators—the program focuses not only on restoring function but also on empowering patients to adapt and thrive. Providers from UofL Physicians – Physical Medicine & Rehabilitation, part of the UofL Health – Brain & Spine Institute, work closely with each patient to develop personalized plans that support both recovery and long-term quality of life.
If you or someone you know may have sustained a spinal cord injury, seek immediate medical attention by calling 911. UofL Health offers seven Emergency Departments, open 24/7 and staffed by experts in trauma and neurological care.
To learn more about the Spinal Cord Program or to schedule a consultation, call 502-582-7400.









